ARES Research Projects
The ARES program has been in operation for over 20 years. The main objectives are to implement innovative strategies to improve healthcare quality and patient safety. The program works with academic partners to create new knowledge through collaborative research that leads to the prevention of healthcare-associated infections (HAIs), antibiotic resistance, and other adverse health outcomes. Read more about our projects on the pages below.
Antibiotic Stewardship
PI: Lauren Dutcher and Keith Hamilton
Study dates: 6/1/21 –5/31/23
Funding source: CDC Prevention Epicenters Program
Area of focus:
Natural language processing for antibiotic prescribing in sinusitis
Specific Aim 1:
Sub-Aim A: To develop a natural language processing (NLP)algorithm to determine appropriateness of antibiotic therapy for adultpatients with acute sinusitis.
Sub-Aim B: To validate and evaluate performance characteristics of the adult sinusitis NLP algorithm. Hypothesis:An NLP algorithm to determine appropriateness of antibiotic therapy for sinusitis in adults will be associated with high accuracy.
Specific Aim 2:
Sub-Aim A: To develop an NLP algorithm to determine appropriateness of antibiotic therapy for pediatricpatients with acute sinusitis.
Sub-Aim B: To validate and evaluate performance for the pediatric sinusitis NLP algorithm.Hypothesis:An NLP algorithm to determine appropriateness of antibiotic therapy for sinusitis in pediatric patients will be associated with high accuracy.
Starting in Q3
Funding Source: CDC Prevention Epicenter Program
Title: The Communication And Coaching To Increase Steward Influence (CACTIS) Intervention to Maximize the Effectiveness of Post Prescription Review with Feedback: A Pilot Feasibility Study
Area of Focus:
It is well-established that antimicrobial stewardship programs (ASPs) can reduce unnecessary antimicrobial use, decrease adverse drug events, and improve patient outcomes, such as reducing Clostridioides difficile infections. However, a critical research gap exists in the identification of strategies to implement and sustain evidence-based ASP interventions such that their full benefits across settings are realized. Studies have demonstrated the importance of face to face communication in ASP, but none have evaluated ways to increase the effectiveness of the way ASP personnel communicate on prescriber acceptance of interventions to optimize antimicrobial use.
Specific Aims:
The goal of this study is to evaluate the feasibility, acceptability, and preliminary impact of an ASP personnel-directed communication and coaching intervention to increase prescriber acceptance of post-prescription review with feedback (PPRF) recommendations. The project has three aims:(1)To optimize the Communication and Coaching to Increase Steward Influence (CACTIS) intervention via a collaborative expert stakeholder panel drawn from the CDC Epicenters Working Group (2) To determine the feasibility and acceptability of the CACTIS intervention to ASP personnel(3) To explore the impact of the CACTIS intervention on rates of prescriber acceptance of PPRF recommendations to discontinue, deescalate or change the duration of an antimicrobial prescription. Our long-term goal is to use the findings of this study to inform a large multisite stepped-wedge cluster-randomized trial to test hypotheses about the effects of the CACTIS intervention on acceptance of PPRF, antimicrobial appropriateness, and patient outcomes.
PI: Ebbing Lautenbach, MD, MPH, MSCE
Study dates: 08/01/21 –07/31/23
Funding source: CDC
Title: Investigating Antimicrobial Stewardship Practices in Southern Africa (MOSAIC)
Area of focus: antibiotic stewardship; global health
Specific Aims:
The goals of this project are 1) To develop survey instruments that measure national-level and hospital-level AS practices, resources, and needs for use in a global context, 2) To conduct a comprehensive survey of AS practices, resources and needs at the national-level and hospital-level across three countries in Southern Africa, 3) To identify national-level and hospital-level contextual barriers and facilitators to the implementation of AS in Botswana and 4) To examine the impact of a stakeholder-engaged capacity building process on knowledge and attitudes towards AS in Botswana.
Adult Project Lead: Lauren Dutcher
Pediatric Project Lead: Kathleen Chiotos
Study dates: 9/1/21 –8/31/23
Funding source: CDC contract
Area of focus:
Use of electronically derived automatic reports of appropriate antibiotic use in stewardship interventions for pharyngitis and community acquired pneumonia
Specific Aims:
1.Use automated reports to assess appropriateness of antibiotic use for: 1) adult inpatients with community acquired pneumonia (CAP); 2) pediatric inpatients with CAP; 3) adult outpatients with acute pharyngitis; and 4) pediatric outpatients with acute pharyngitis
2.Design and implement a scalable and sustainable antibiotic stewardship feedback reported-based intervention for these four conditions
3.Track the impact of stewardship interventions and report to key stakeholders, including prescribers
4.Create a publicly available toolkit based on the findings of this project that includes: (1) analytic tools and resources for using the automated reports of key indicators to target stewardship interventions and (2) an implementation guide to inform the application of automated reports to stewardship in the inpatient and outpatient settings
N/A- study begins Year 4
PI: Ebbing Lautenbach, MD, MSCE, MPH
Study Dates: 09/01/21 – 08/31/23
Funding Source: CDC
Area of Focus:
Antibiotic Stewardship
Specific Aims:
This project will assess the impact on antibiotic use of previously developed automated reports to identify inappropriate antibiotic prescribing in targeted inpatient and outpatient conditions in adults and children.
Antibiotic Resistance
Study Dates: 2018-2023
Funding Source: NIAID, NIH
Area of Focus:
A study of the genomic characteristics of colonizing intrasubject lineages of S. aureus, how they are impacted by antibiotic use, and which S. aureus evolutionary trajectories and genetic changes are associated with recurrent infections and/or with persistence of body colonization.
PI: Ebbing Lautenbach, MD, MPH, MSCE
Study dates: 07/01/21 – 06/30/22
Funding source: CDC
Area of focus:
Global antibiotic resistance; MDROs; Whole genome sequencing
Specific aims:
The goals of this project are to 1) Describe the genetic diversity of circulating hospital and community ESCrE and CRE in Botswana and put in context of global strain collections, 2) Evaluate evidence of household/community transmission among ESCrE and CRE colonized individuals, and 3) Characterize the structure and prevalence of mobile elements harboring resistance determinants of interest.
PI: Ebbing Lautenbach, MD, MPH, MSCE
Study dates: 06/01/18 – 05/31/23
Funding source: NIH
Specific Aims:
Aim 1: To identify risk factors for colonization or infection with colR-CRE in LTACH patients; Aim 2: To evaluate the impact of colR-CRE colonization or infection on mortality in the LTACH setting; Aim 3: To use whole-genome sequencing to prospectively evaluate colR-CRE isolates from a regional network of LTACHs with a high baseline prevalence of CRE.
Study Dates: 06/01/23 – 12/31/25
Funding Source: CDC Prevention Epicenter Program
Area of Focus:
Environmental transmission of pathogens; healthcare-associated infection
Specific Aims:
This project aims to define high-touch objects and to determine effectiveness of cleaning within inpatient NEXUS areas including dialysis, radiology, and physical and occupational therapy
Study Dates: 12/1/2016 – 11/30/2018
Funding Source: Antibacterial Resistance Leadership Group / NIH
Area of Focus:
MDROs; Solid Organ Transplantation
Specific Aims:
1. To elucidate risk factors for ESBL-EB bloodstream infection among SOT recipients. 2. To determine the impact of ESBL-EB bloodstream infection on time to mortality in SOT recipients. 3. To describe the phenotypic and genotypic characteristics of ESBL-EB causing bloodstream infections in SOT recipients
Healthcare Associated Infections & Infection Prevention
Study Dates: 06/01/21 – 05/31/26
Funding Source: CDC
Areas of Focus:
Healthcare-associated infections; C. diff
Specific Aims:
1. Determine the impact of the Screening and Targeted Prophylaxis (SToP) protocol on risk of in-hospital and 90-day CDI among subjects admitted for SOT, HCT, or induction chemotherapy. 2. Determine the impact of the SToP protocol on risk of in-hospital and 90-day VRE infection among subjects admitted for SOT, HCT, or induction chemotherapy. 3. Determine the risk factors for C.difficile colonization among subjects admitted for SOT, HCT, or induction chemotherapy
PI: Matthew Ziegler, MD, MSCE
Study Dates: 02/01/2020 – 12/31/2025
Funding Source: NIH / NIAID
Title: Impact of Early Gut Microbiome Features on Risk of Neutropenic Fever and Bloodstream Infection in Hematologic
Area of Focus: Healthcare-associated Infection; Immunocopromised; Oncology
Specific Aims: This project aims to identify predictors of neutropenic fever and bloodstream infections among patients receiving treatment of hematologic malignancy through longitudinal assessment of the gut microbiome and measures of mucosal integrity and inflammation.
PI:
Study Dates:
Funding Source:
Title:
Area of Focus:
Specific Aims:
PI: Ebbing Lautenbach, MD, MPH, MSCE
Study Dates: 12/31/20 – 12/30/21
Funding Source: NA
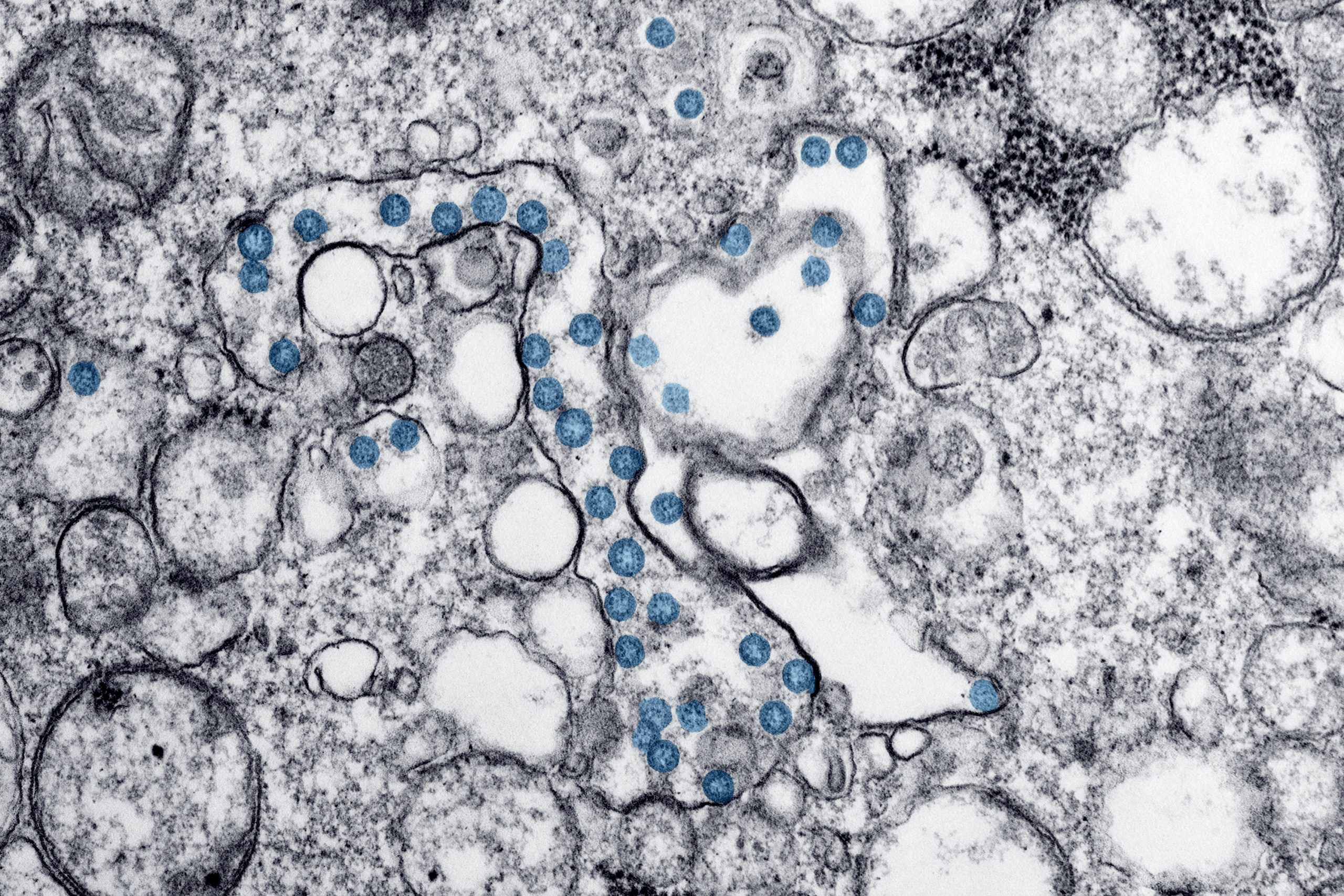
Area of Focus: Healthcare-associated infection; COVID
Specific Aims: This project addresses the epidemiology of, and risk factors for, secondary infection and multidrug-resistance organism colonization and infection in long term acute care hospital patients with recent COVID-19 infection.
Site PI: David Pegues, MD
Study dates: 4/2019-3/2023
Funding source: AHRQ
Area of focus:
Prevention of healthcare-associated bloodstream and access device-associated infections among hemodialysis patients
Specific Aims:
Aim 1: Assess whether nasal povidone-iodine decolonization reduces infections among hemodialysis patients using a multicenter, stepped-wedge cluster randomized trial.
Aim 2: Evaluate patient satisfaction with nasal povidone iodine decolonization, assess its role in patient activation, and assess barriers and facilitators to implementation using patient surveys.
Aim 3: Examine healthcare worker satisfaction with implementation of nasal povidone-iodine decolonization and assess barriers and facilitators to the process via qualitative interviews and site visits.
Study Dates: 4/01/2017 – 06/30/2020
Funding Source: Gift of Life Donor Program
Area of Focus:
Opioid epidemic; MDROs; solid organ transplantation; donor-derived infections
Specific Aims:
1. Determine the impact of injection drug use among organ donors on donor culture positivity.
2. Determine the impact of injection drug use among organ donors on risk of post-transplant recipient infection.
PI: Ebbing Lautenbach, MD, MPH, MSCE
Study Dates: 06/01/21 – 05/31/26
Funding Source: CDC
Area of Focus:
Healthcare-associated Infections; Microbiome Research; C. Diff;
Specific Aims: The projects proposed in this application seek to build on the strong foundation established by core and collaborative projects conducted by the Penn-CHOP investigators over the past 5 years.
Sociobehavioral and Implementation Science
Funding Source: CDC Prevention Epicenter Program
Area of Focus:
It is well-established that antimicrobial stewardship programs (ASPs) can reduce unnecessary antimicrobial use, decrease adverse drug events, and improve patient outcomes, such as reducing Clostridioides difficile infections. However, a critical research gap exists in the identification of strategies to implement and sustain evidence-based ASP interventions such that their full benefits across settings are realized. Studies have demonstrated the importance of face to face communication in ASP, but none have evaluated ways to increase the effectiveness of the way ASP personnel communicate on prescriber acceptance of interventions to optimize antimicrobial use.
Specific Aims:
The goal of this study is to evaluate the feasibility, acceptability, and preliminary impact of an ASP personnel-directed communication and coaching intervention to increase prescriber acceptance of post-prescription review with feedback (PPRF) recommendations. The project has three aims:(1)To optimize the Communication and Coaching to Increase Steward Influence (CACTIS) intervention via a collaborative expert stakeholder panel drawn from the CDC Epicenters Working Group (2) To determine the feasibility and acceptability of the CACTIS intervention to ASP personnel(3) To explore the impact of the CACTIS intervention on rates of prescriber acceptance of PPRF recommendations to discontinue, deescalate or change the duration of an antimicrobial prescription. Our long-term goal is to use the findings of this study to inform a large multisite stepped-wedge cluster-randomized trial to test hypotheses about the effects of the CACTIS intervention on acceptance of PPRF, antimicrobial appropriateness, and patient outcomes.
Funding Source: Society for Healthcare Epidemiology of America (SHEA) Research Scholar Award
Area of Focus:
Hospital-based initiatives dedicated to improving the use of antibiotics, known as Antimicrobial Stewardship Programs (ASP), have been demonstrated to improve the quality of patient care and reduce harm.Despite this, the uptake and implementation of ASPs in US hospitals has been incomplete and inconsistent. There is an urgent need to understand how evidence-based ASP interventions can be tailored to and sustained within hospitals, based on existing needs, available personnel and other contextual factors. ASP personnel, traditionally physicians and pharmacists with infectious diseases training, play a critical role in the successful implementation of ASP interventions. In addition to providing expert guidance, they promote improvement through communication and engagement with prescribers. In achieving these goals, ASP personnel are faced with a number of challenges including lack of time, lack of financial resources, resistant prescribers, an overwhelming workload, insufficient information technology and lack of leadership support. These conditions may contribute to burnout, a syndrome characterized by depersonalization, emotional exhaustion and a diminished sense of personal accomplishment. Previous research has demonstrated that, in general, infectious diseases physicians and pharmacists experience a significant degree of burnout. However, there has been no research to date on burnout in ASP personnel specifically. Burnout in this group may lead to frequent turnover and diminished capacity to engage prescribers to improve antibiotic use, thus limiting the impact of ASP interventions.
Emerging Pathogens & Novel Therapeutics
Study Dates: 2018-2023
Area of Focus: We will determine the frequency of likely transmission of MRSA leading to bacteremia in the hospital and to assess for bacterial genetic markers of poor outcomes in patients with MRSA bacteremia.
Specific Aims:
1. Compare the genomes of all infecting MRSA isolates to assess for genomic clustering of MRSA bacteremia isolates, suggesting local spread of one or more MRSA strains in the hospital or in the community.
2. Determine clinical and genomic risk factors for 30-day mortality among MRSA patients.
3. Assess which (if any) genomic factors (e.g., presence of mobile genetic elements, agr dysfunction, strain type) are associated with 30-day mortality or complications of bacteremia.
4. Determine how often recurrent MRSA bacteremia is caused by a single clonal strain and how often a recurrence is caused by a new strain of MRSA.
Microbiome Research, Transmission Studies & Environmental Studies
Study Dates: 06/01/23 – 12/31/25
Funding Source: CDC Prevention Epicenter Program
Area of Focus:
Environmental transmission of pathogens; healthcare-associated infection
Specific Aims:
This project aims to define high-touch objects and to determine effectiveness of cleaning within inpatient NEXUS areas including dialysis, radiology, and physical and occupational therapy
PI: Ebb Lautenbach, MD, MSCE, MPH
Project Lead: Katie Chiotos
Study Dates: 6/1/2021-5/31/2026
Funding Source: Centers for Disease Control and Prevention
Area of Focus:
Respiratory microbiome, ventilator-associated pneumonia diagnostics, multidrug resistant organisms
Specific Aims:
Aim 1: To determine the longitudinal changes in LRT and GI alpha diversity attributable to antibiotic class exposure.
Aim 2: To determine the impact of LRT and GI dysbiosis on diagnosis of LRTI.
Aim 3: To determine the association between LRT and GI dysbiosis and MDRO and/or other bacterial colonization.
PI: Brendan Kelly, MD
Study Dates: 06/01/21 – 05/31/26
Funding Source: CDC
Area of Focus:
Healthcare-associated Infections; Microbiome Research; C. Diff;
Specific Aims: The projects proposed in this application seek to build on the strong foundation established by core and collaborative projects conducted by the Penn-CHOP investigators over the past 5 years.